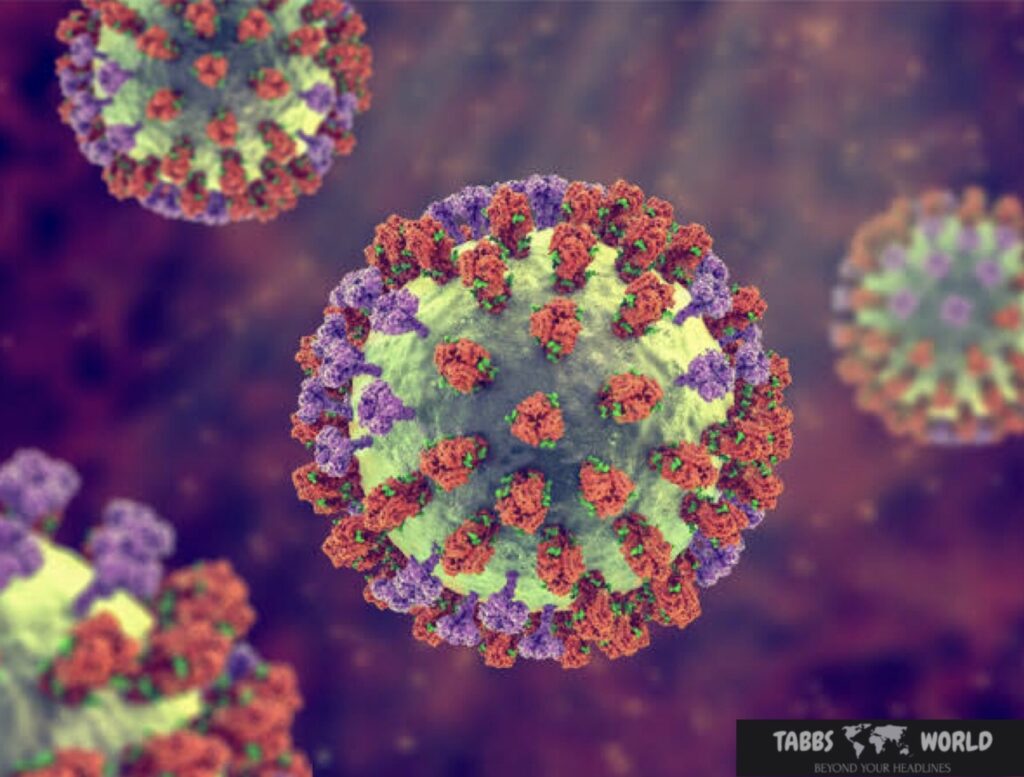
As we approach the start of the 2024-2025 flu season in the Northern Hemisphere, health care officials are gearing up to tackle the perennial challenge of influenza. In the ongoing battle against this ever-evolving virus, updated guidance on vaccine formulation is critical to increasing protection and reducing the impact of influenza-related morbidity and mortality.
Each year, influenza viruses undergo genetic changes, requiring adjustments in vaccine formulation to ensure maximum efficacy. The World Health Organization (WHO), in collaboration with global health experts, continuously monitors influenza virus activity and recommends updating vaccine formulations to match circulating strains.

Understanding influenza virus:
dynamics Influenza viruses are notorious for their ability to mutate rapidly, leading to the emergence of new strains with varying degrees of virulence and transmissibility. The main types of influenza viruses that cause seasonal flu in humans are influenza A and B viruses. Influenza A viruses are further classified into subtypes based on two surface proteins: hemagglutinin (H) and neuraminidase (N).
The continued evolution of influenza viruses poses a formidable challenge to public health efforts, requiring vigilance and adaptation in vaccine development strategies. Each flu season presents a unique set of conditions, with the potential for new strains to emerge and spread within communities.
Guidance for vaccine formulation:
Influenza vaccine formulation is a complex process involving the selection of strains likely to predominate during the coming flu season. This decision is informed by surveillance data collected from around the world, including information on the genetic characteristics and antigenic characteristics of circulating influenza viruses.
For the 2024-2025 flu season, WHO has issued updated guidance on vaccine formulation based on comprehensive analysis and assessment of influenza virus activity. The recommendations aim to improve vaccine effectiveness by aligning composition with the most prevalent and antigenically distinct strains circulating in the Northern Hemisphere.
Guidance issued by the WHO for the 2024-2025 flu season emphasizes several key considerations in influenza vaccine formulation:
1: Antigenic characteristics:
Stringent antigenic characterization of influenza viruses is essential to identify strains that are likely to evade immune recognition and cause significant disease. By analyzing the antigenic characteristics of circulating strains, researchers can prioritize the selection of vaccine components that elicit strong immune responses.
2: Genetic analysis:
Genetic sequencing provides valuable insight into the evolutionary dynamics of influenza viruses, enabling scientists to detect the emergence of new variants and assess their potential impact on vaccine effectiveness. Close monitoring of genetic changes helps inform decisions regarding strain selection and vaccine formulation.
3: Hemispheric variation:
Influenza virus circulation varies between the northern and southern hemispheres, with distinct seasonal patterns and dominant strains observed in each region. Although surveillance data from the Southern Hemisphere can inform vaccine formulation decisions for the Northern Hemisphere, regional differences in virus activity should be considered with caution.
4: Targeted Protection:
Vaccination is the most effective strategy for preventing influenza-related illness and its complications. By targeting the strains most likely to cause illness in the coming flu season, influenza vaccines can provide individuals with the best possible protection against infection and associated morbidity and mortality.

Challenges and opportunities:
Despite advances in vaccine technology and surveillance capabilities, many challenges remain in the fight against influenza. The emergence of new strains, the potential for vaccine mismatches, and vaccine hesitancy are among the factors that complicate efforts to control the spread of the virus.
However, ongoing research and collaboration within the global health community provides opportunities to address these challenges and improve influenza prevention and control strategies. Innovations in vaccine development, such as the use of novel adjuvants and delivery systems, hold promise for increasing vaccine efficacy and broadening immune protection.
Additionally, public awareness campaigns and educational initiatives play an important role in promoting influenza vaccination and dispelling myths about vaccine safety and efficacy. By promoting a culture of influenza prevention and immunization, communities can reduce the burden of flu-related illness and protect public health.
results:
As we prepare for the 2024-2025 flu season in the Northern Hemisphere, updated guidance on influenza vaccine formulation underscores the importance of proactive measures to combat this perennial public health threat. By leveraging surveillance data, genetic analysis, and scientific expertise, health care officials can improve vaccine effectiveness and reduce the impact of influenza-related morbidity and mortality.
Ultimately, meeting the challenges posed by influenza requires a collective effort to ensure that individuals and communities are adequately protected against this infectious disease. Through continued research, innovation, and public health interventions, we can strive toward a future where the burden of influenza is minimal, and the benefits of vaccination are known to all.
Table of Contents
Why is there a need for updated guidance on influenza vaccine formulation each year?
Influenza viruses undergo constant genetic changes, leading to the emergence of new strains. To ensure optimal protection, vaccine formulations must be adjusted annually to match the predominant circulating strains.
Who provides guidance on influenza vaccine formulation for each flu season?
The World Health Organization (WHO) collaborates with global health experts to monitor influenza virus activity and make recommendations on vaccine compositions for the upcoming flu season.
What factors are considered when formulating influenza vaccines?
Key considerations include antigenic characterization of circulating strains, genetic analysis to track viral evolution, hemispheric variability in virus activity, and the potential for vaccine mismatches.
How are influenza vaccine components selected for inclusion in the seasonal vaccine?
Surveillance data, genetic sequencing, and antigenic analysis inform the selection of vaccine components, with a focus on strains likely to cause illness during the upcoming flu season.
Why is it important to monitor influenza virus activity in both the Northern and Southern Hemispheres?
Influenza viruses circulate seasonally in both hemispheres, with distinct patterns and predominant strains observed in each region. Surveillance data from the Southern Hemisphere can help anticipate which strains may circulate in the Northern Hemisphere during its flu season.
How effective are influenza vaccines in preventing illness?
Influenza vaccines are typically 40% to 60% effective in preventing illness when the vaccine strains closely match the circulating strains. Even when mismatches occur, vaccination can still reduce the severity of illness and complications.
What can individuals do to protect themselves and others from influenza?
In addition to vaccination, individuals can reduce their risk of influenza by practicing good hand hygiene, covering coughs and sneezes, avoiding close contact with sick individuals, and staying home when ill to prevent the spread of the virus.